There has never been a more relevant time to discuss patient experience in healthcare. Patients can articulate, better than ever before, their preferences and needs, and different healthcare strategic documents require patient and public involvement to ensure the service provided meets the needs of its intended audience and service users.1 The rise of the “expert patient”, a person who is expert by “lived experience” is changing how we do medical imaging and other aspects of patient care.2,3 Furthermore, many research projects and funding applications now require direct patient engagement in all aspects of the project pipeline, to ensure “everything about the patients is designed by them and with them.”4,5
Therefore, the following aspects of patient experience will be covered in this blog:
-
What is the importance of patient positioning in the overall patient experience?
-
Which conditions should be met for an ideal positioning of the patient?
-
What direct Influence can Radiographer have on the Patient Experience?
Importance of patient positioning

One of the most central areas affecting patient experience in radiology and radiography, excluding the communication between healthcare professionals and patients, is patient positioning.6-8
Positioning is the act of preparing the patient to undertake a medical imaging examination, in order to expertly delineate the required anatomy and pathology, while keeping patients safe and comfortable and it is vital for so many aspects of patient experience but also patient outcomes. It can involve the positioning of the whole-body anatomy in relation to the image receptor (anterior posterior, posterior anterior, supine, prone or decubitus, for instance) but also in relation to the examination table9 and/or the positioning of a particular body area to facilitate imaging with the use of positioning aids e.g., immobilisation of elbow or knee joint.
There is now a wealth of positioning aids available to achieve this, each one with its own merits and challenges. There are foam pads, pillows, beaded support systems, hoists, wedges in all shapes and sizes, to name just a few. Positioning can be an intimate task, as it often involves “touching” the patient to explain and show how to lie down on the imaging equipment or to move them if needed to a different position for the examination. Many patients often said that this is the part of the examination that mostly “stays with them” as it is an opportunity for human interaction with another person at a time they feel at their most vulnerable.10
Requirements for Optimal positioning aids
-
Positioning aids need to be safe and not creating any additional risks for staff or patients; this might also include that it will not warm up during the examination (which might create risk of burns) or interact in any other way with the medical imaging equipment (attracted or repelled by it, such as, for instance, in MRI projectile events) or inadvertently increase radiation dose for any examination (e.g., CT examinations)
-
Positioning aids need to be cleanable for infection control (more relevant now than ever, given additional measures introduced to prevent cross-infection from contagious or infectious diseases, including Covid-19)
-
Positioning aids also need to be compatible with imaging (not overlapping with patient anatomy or pathology) and complying with the imaging principles of each imaging modality, to avoid creating image artefacts that may impact the imaging outcome of the examination. An example herefore are materials with high susceptibility, that can disrupt the magnetic field in MRI, or materials that can create a shadowing artefact in ultrasound or absorb x-rays are to be avoided as positioning tools, as they disrupt the process of image creation.
-
Ideally positioning aids need to be flexible or mouldable, to ensure it can assume the shape or size needed for each patient, to customise and personalise their positioning.
Radiographer’s impact on patient experience 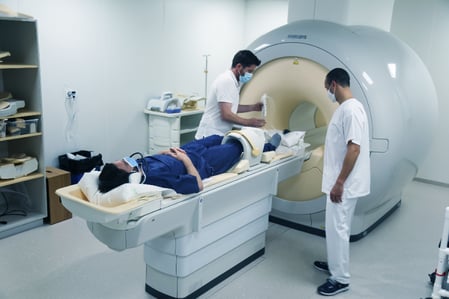
In the vast majority of the cases the person responsible for patient positioning in medical imaging and treatment planning within radiology is the radiographer, also known as medical radiation technologist (MRT). While the principle of radiographic positioning is formally taught in all undergraduate radiography programmes, it also takes quite some practice and experience over time for this skill to be refined and perfected; radiographers often need to be quite resourceful in the use of patient positioning equipment and innovate “on the spot” to customise to their patient needs every time, as required, to delineate the anatomy and pathology of the treatment.
CONCLUSION
It is hard to measure, how big the influence of these factors is on the patient experience. But it is widely known that a good patient experience is correlated with patient positioning, the equipment used for the positioning and the radiographer itself also influences the patient experience through the interaction with the patient.
Credits to: Dr Christina Malamateniou, PhD (MRI), MA (Clinical Education), DIC, MAcadMEd, BSc Hons, SFHEA.
About PEARL TECHNOLOGY
Pearl Technology AG, based in Schlieren, offers innovative solutions for the placement, positioning and immobilization of patients in radiology and radiotherapy. The products are manufactured in Switzerland according to ISO norm 13485 and are characterized by simple handling, high patient comfort and excellent hygiene which guarantees smooth and safe examination processes.
Download further information on our patient positioning portfolio for radiology and nuclear medicine or contact us directly in order to receive further information on our patient positioning solutions.
List of references
1. Patient Public and Practitioner Partnerships within Imaging and Radiotherapy: Guiding Principles (SCoR, September 2018)
2. Edgar A. The expert patient: Illness as practice. Med Health Care Philos. 2005;8(2):165-71.
3. Tyreman S. The expert patient: outline of UK government paper. Med Health Care Philos. 2005;8(2):149-51
4. Gremyr A, Andersson Gäre B, Thor J, Elwyn G, Batalden P, Andersson AC. The role of co-production in Learning Health Systems. Int J Qual Health Care. 2021 Nov 29;33(Supplement_2):ii26-ii32.
5. NIHR guidelines for patient and public involvement (2022) https://www.nihr.ac.uk/documents/ppi-patient-and-public-involvement-resources-for-applicants-to-nihr-researchprogrammes/23437 (accessed July 1st 2022)
6. Boyd LL, Clark KR. Reducing Pediatric Patients’ Dose by Manipulating Radiographic Projections. Radiol Technol. 2021 Nov;93(2):150-160.
7. Cuccia F, Alongi F, Belka C, Boldrini L, Hörner-Rieber J, McNair H, Rigo M, Schoenmakers M, Niyazi M, Slagter J, Votta C, Corradini S. Patient positioning and immobilization procedures for hybrid MR-Linac systems. Radiat Oncol. 2021 Sep 20;16(1):183.
8. Elmaoglu M, Celik A, MRI handbook: MRI Physics, patient positioning and protocols, Springer, NY, 2012
9. Radiopaedia website on radiographic positioning terminology https://radiopaedia.org/ articles/radiographic-positioning-terminology?lang=gb (accessed July 6th 2022)
10. Lloyd L. A Tale of Two MRIs. J Med Imaging Radiat Sci. 2020 Dec;51(4S):S9-S10.

